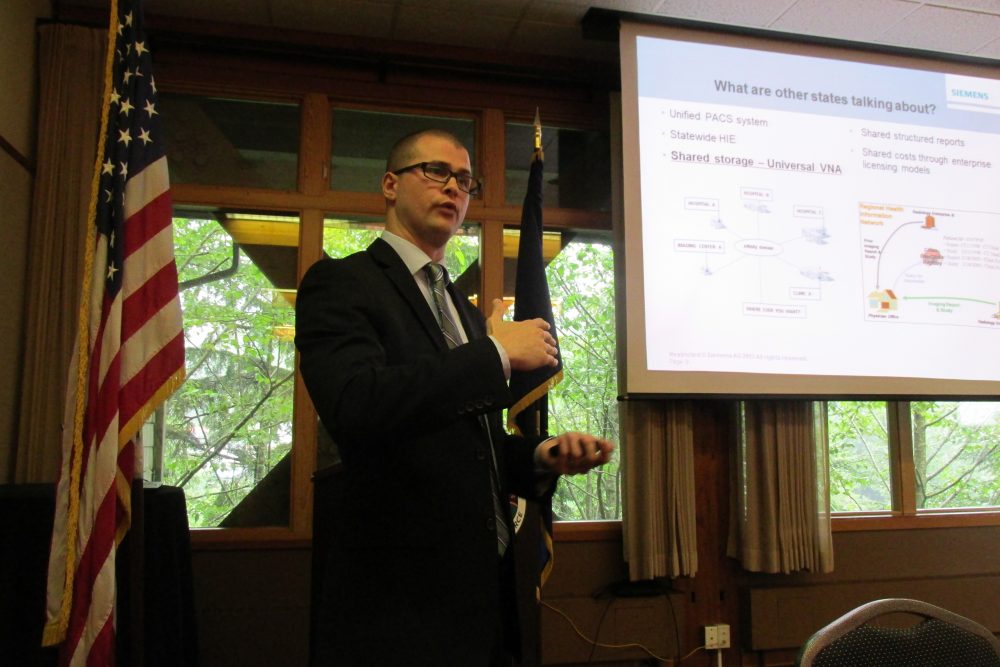
What is the future of healthcare, and how can you create and maintain positive medical trends in the community? That was the topic of discussion at Wednesday’s Ketchikan Chamber of Commerce luncheon.
Logan Mcmackin is a computer specialist working in the Pacific Northwest for Siemens. Mcmackin spoke about technology used to improve efficiency and communication in the medical field.
He says an incentive program was put into place several years ago to encourage digitalization of health records. In addition, he says under the Affordable Care Act, the trend is shifting to the Merit-Based Incentive Program, also known as MIPS.
“Basically what they did was they took all the incentive programs out there – Meaningful Use, which is making things digital; the Physician Quality Reporting System; the Value-Based Payment Modifier. They added a new section – Clinical Improvements. They bundled all of those under the MIPS program.”
He says each of the categories is given a different weight, which determines how much a medical provider will be reimbursed by the federal government.
Mcmackin says another form of reimbursement is through an alternative payment model or APM. He says these are used by more progressive groups such as patient-centered medical homes.
“Basically what it means is that they are getting bundled payments for treating a disease state, and they’re also going ‘at risk’ for that. And depending on how well and effectively I treat that, I can either make a bunch of money or I can potentially lose money.”
He says that demonstrates the shift from a fee-for-service model, in which payments are made based on the number of services provided, to value-based care. Value-based care is designed around the patient and works to improve the patient’s overall health.
Mcmackin also discussed the Alaska eHealth Network. This healthcare information exchange, or HIE, allows physicians and providers access to a patient’s medical records statewide.
“So, if I’m a provider and I’m sitting in an emergency room and I have somebody that was in a motor vehicle accident come in, who’s unconscious, I don’t have access to their patient records. I don’t know what exams they’ve done. I don’t have any information on their medical history. But if that patient is part of this HIE, I can now pull them up and see everything that they’ve had done at any facility.”
Mcmackin says, in Alaska, the electronic network is mainly used to share images and radiology reports. He says it also can be used to share laboratory and pharmacy information, and determine if a patient is going to multiple providers for medications. Mcmackin says electronic records improve efficiency because all providers have access to the same records, reducing the need for consultations, or time spent going through paper records.
Mcmackin mentioned trends in other states, including a vendor-neutral archive where all hospitals’ records are in a shared database.
Another trend is shared-structure reporting. McMackin says a single reporting format makes it easier for providers to find information when receiving records from another medical office.
“But all of the reports that they’re going to be getting funneled into them will be identical to the reports that their cardiologists are doing. So now I’m not spending three minutes reading through a report trying to find the information I want or getting a report that doesn’t have the information I want. I know exactly where it is because it’s identical to the ones that I’m doing all day long.”
Mcmackin also spoke about how data from electronic medical records can be used, such as determining how much time is spent on procedures, and reporting. He says this information can be used to improve efficiency. Patient data can be analyzed to determine population health statics as well as lifestyle and behavioral health habits. Mcmackin says the ultimate goal is to improve health, lower costs and provide better care.